QI Celebrates Opening of New Brain Imaging Facility
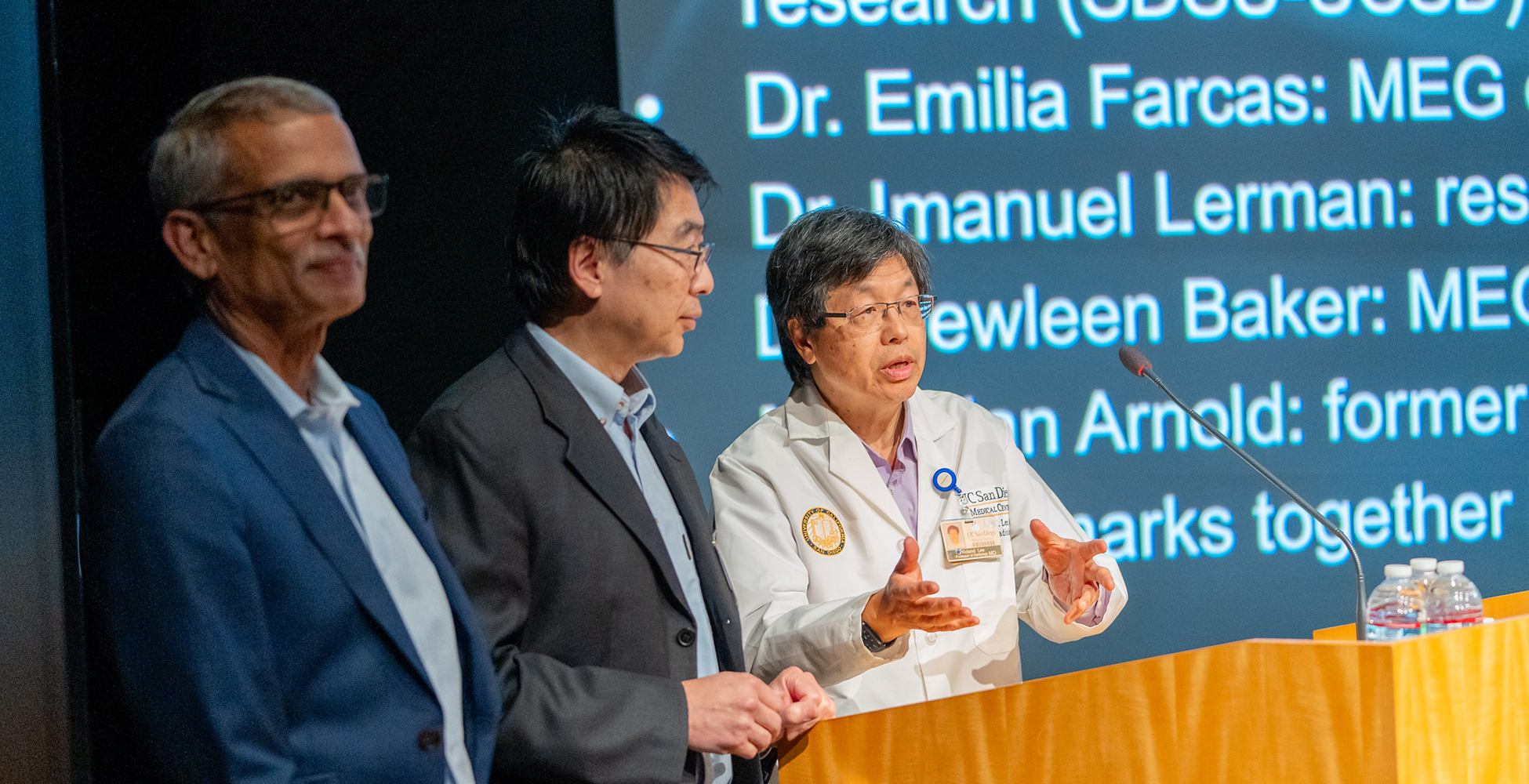
On December 7, 2023, the Qualcomm Institute (QI) held an open house and symposium celebrating its new Magnetoencephalography (MEG) Center, which offers the most advanced and accurate noninvasive functional brain imaging technique currently available. Guests had the opportunity to tour the facility, which will support both research and clinical activity for users across Southern California.
Here are excerpts (edited for clarity) from the event’s distinguished speakers.
“This day, the seventh of December, has special meaning for those of us who have been part of the California Institute for Telecommunications and Information Technology, whose UC San Diego division is the Qualcomm Institute, because 23 years ago—to the day—is when we were established with a $100 million dollar award from the state of California, which had to be matched with $200 million from non-state sources… The vision behind it was to create unique research facilities that you couldn’t create in your own labs, but that would be a shared resource for everybody, not only on campus, but also off campus… I have to admit we did not have the MEG in mind at the time. But we never interpreted the founding focus as something that constrains and limits, but as an exemplar of what we should be doing into the future.”
—Ramesh Rao, director of QI, UC San Diego

“One of the real goals of this institute [QI] is to be a broad transdisciplinary institute that has significant impacts on the campus across the whole spectrum, from the arts to the hospital and everywhere in between. And the MEG is … one of the ways that we can support, in this case, cutting-edge research and clinical instrumentation in a central location on the campus. It’s really state-of-the-art. I was told there’s only maybe two of these in all California. And so I’m really pleased that we were able to work through all the red tape to get it moved from Sorrento Valley up here.”
—Robert Continetti, senior associate vice chancellor of academic affairs, UC San Diego

“One of the first things that my lab did with the [MEG] tool was to look at a memory retrieval signal. There was a debate going on about this parietal signal that was taking place when you remembered something. They didn’t know whether it was a rumination on the materials that you just retrieved, or whether it was a search for an internal memory engram. Bioengineering graduate students worked with me and really helped me answer that question using the increased time sensitivity of MEG. So that just shows the power of this tool. The other thing it really demonstrates is that UC San Diego has such a wealth of cross-disciplinary expertise.”
—Jim Brewer, chair, Neurosciences, School of Medicine, UC San Diego

“I can tell you personally that this MEG has actually helped me keep patients safer. [MEG Center Director] Roland [Lee] has always in his time in neuroradiology been very gracious about putting together beautiful integrated PowerPoints that actually showed me and my patients precisely where different areas of eloquence were. That allowed me to have very informed discussions with individual patients, not based on generalized structural atlases, but based on their particular stimulation profiles of the risk of a transcortical approach to their lesion. You can’t imagine the relief that’s brought individual patients, but more importantly how it stimulated my own thinking and the thinking of other researchers in our department of how we can actually better define structural targets in conditions that currently aren’t managed by neurosurgeons.”
—Alexander Khalessi, chair, Neurological Surgery, School of Medicine, UC San Diego

“MEG is one of the emerging techniques to be able to ascertain what treatment targets we need to both understand psychiatric conditions, but also to understand a treatment. So this is an example of really making sure that we can identify deep brain regions—not only identify them anatomically, but understand key physiological functioning… With technology like MEG, we’re better able to reconcile the complex anatomy and the complex physiological signaling, and how that interacts with both the disease and how it better interacts with treatment interventions for severe psychiatric illnesses including depression.”
—Zafiris “Jeff” Daskalakis, chair, Department of Psychiatry, School of Medicine, UC San Diego
“We always talk about translational medicine. Well, this is a true example of that. Because [MEG Center Co-Director] Mingxiong Huang is one of the world’s best researchers in terms of figuring out how to solve the inverse problem [the process of calculating from the magnetic fields measured by the helmet sensors, the location and time-activity of the brain cells that produced them]. And he creates algorithms that we publish in peer-reviewed articles, and then we implement these for the benefit of our patients. Some of the software he has developed is now licensed by the MEG company, and is used to really help patients. We do clinical MEG for patients with epilepsy and with brain tumors, and concussions, as well as doing research. [This new facility is a] tribute to the people, the support from Qualcomm Institute, from Radiology, from the three chairs who just spoke [Neuroscience/Neurology, Neurosurgery and Psychiatry Departments of UC San Diego School of Medicine], scientists like Tom Liu, the head of the FMRI center, and they are on our board of directors.”
—Roland Lee, director of MEG Center, QI, UC San Diego; also emeritus professor of radiology, School of Medicine, UC San Diego, and physician with Veterans Affairs (VA) San Diego Healthcare System
“We had to tear apart the 6-layer magnetic shielded room in the old site into modules. And then [three engineers] came over to QI and reset up this big, 26 metric ton shielded room at QI… Ramesh [Rao] and team allowed us to knock down a whole bunch of drywalls to make the space for us… The door and also the walls of the shielded room are two feet thick… For the most part, the performance of the shielded room is amazing. This is probably one of the best rooms in the world for MEG… [For principal investigators running] pilot projects to get some pilot data from your next NIH RO1 MERIT grant, we offer a huge discount… For junior faculty [applying for certain career development grants, such as NIH K-award or VA CDA award], we offer a further discount. Please contact us. We’re always here to serve you.”
—Mingxiong Huang, co-director of MEG Center, QI, UC San Diego; adjunct professor in the UC San Diego Electrical and Computer Engineering (Jacobs School of Engineering) and Radiology Departments (School of Medicine); and scientist with VA San Diego Healthcare System
“We have the best MEG room and instrument in the world. And we have the best group of people working on it. So I think we could use more people coming and using it, especially from the upper campus… [With MEG] you are recording, instantaneously, the currents entering the apical dendrites of the pyramidal cells in the brain you’re recording from. This is amazing. With fMRI, you’d get delay, like two to 10 seconds… [With MEG], you see in real time the synaptic activity of the brain, the cortex… fMRI is noninvasive, but it’s loud and kind of scary; MEG is totally silent, totally noninvasive, totally harmless… [Localization of distributed sources] is something that’s an area of research, and engineers would be welcome.”
—Eric Halgren, professor, radiology, School of Medicine, UC San Diego

“QI has an internship program, which is called mHealth Workforce Initiative. It’s is led by [QI Principal Development Engineer] Ganz [Chockalingam], and it has a one- to two-year internship for undergraduate students who are designing and developing a real-world application in healthcare. So this program is really valuable. It gives them an advantage in future graduate studies or in future job placement … The students are working on two useful projects analyzing MEG data. The first one is detecting epileptic spikes from MEG scans. Currently, this is a manual process where a very specialized analyst manually inspects the scans, and it takes about 10 to 20 hours per one-hour recording of a patient… The students are developing a neural network model that automates the detection process. So this can really have an impact in speeding up the clinical workflow. Another useful project is detecting post-traumatic stress disorder [PTSD] or traumatic brain injury [TBI] from EEG or MEG scans. The students are developing machine learning models that can classify scans as healthy control or PTSD or TBI.”
—Emilia Farcas, associate research scientist, QI, UC San Diego

“We use the magnetic shielded room to do a lot of brain research. Our particular project that was funded through BARDA [Biomedical Advanced Research and Development Authority] and DARPA [Defense Advanced Research Projects Agency] essentially was looking at differences between individuals, most specifically looking at people that may have differences in their immune configuration that causes an inflammatory cascade, to either proliferate and have good or bad outcomes… We do quite a bit of work looking at mental health disorders and how these mental health disorders modify reflexes that change inflammation in the periphery as well as in the brain… We wouldn’t be able to do [our research] without the shielded room and the support from Mingxiong [Huang], Ramesh [Rao].”
—Imanuel Lerman, professor in UC San Diego’s Electrical and Computer Engineering (Jacobs School of Engineering) and Anesthesiology Departments (School of Medicine)
“There’s no diagnostic measure… to truly, objectively diagnose TBI. The MRI and the CT are particularly poor at being at being able to positively diagnose mild TBI … Advances have been made through the research that’s been done by the [MEG] team… In 2014, a paper came out that showed delta-wave slowing… in a rather a good-sized group of healthy controls and folks with TBI, both blast and non-blast TBI. Through analysis of the data, Dr. Huang was able to show… very good sensitivity and specificity in terms of distinguishing TBI from not. And what’s very special about the MEG is the MEG is able to detect individual injury. The slow waves can be seen in the part of the brain where the injury occurs, and that’s different for each patient. There’s an earlier paper in which it was shown that, [in] somebody with somewhat more acute TBI, these waves were present when the symptoms were there and went away when the symptoms began to resolve.”
—Dewleen Baker, professor in residence, psychiatry, School of Medicine, UC San Diego

“I’m 49 years old. Seizures started when I was when I was three. And they just stopped four years ago after a successful laser ablation procedure done through the UCSD Epilepsy Center. The MEG test…was absolutely critical in the diagnosis of one of my seizure foci that wasn’t previously detected when I was doing inpatient video EEG monitoring.”
—Brian Arnold, former MEG patient with epilepsy
Watch one or more of the speakers on QI’s MEG Symposium and Open House video playlist or learn more about the MEG Center on its website.